In addition to the donation of solid organs, for example heart, kidney, liver, lungs and pancreas, it is also possible to donate tissues such as heart valves, skin, veins, bone and connective tissue, corneas and whole eyes. Donated tissues can dramatically enhance the quality of life for recipients, and even save lives.
Unlike organs, human tissue can be processed and stored for an extended period of time for use in burn cases, ligament repair, and bone replacement and, in the case of eye donation, for corneal transplantation and scleral restoration.
In Europe about 20,000 corneal transplantations are performed per year. Unfortunately, about as many patients are currently on waiting lists.
Being a donor means giving consent that, after one’s death, certain organs and tissues may be removed in order to be transplanted to seriously ill people in need of that particular organ or tissue to improve their quality of life, or even save their life.
It is also possible to donate tissues while one is still alive (such as blood, bone marrow, umbilical cord) as well as certain organs in exceptional circumstances (i.e. kidney and parts of liver).
Donating is always free and anonymous. The act of donation is completely voluntarily and can never be performed against the expressed wishes one may have made whilst still alive. The donation of tissue/organs after death is a gift to another person which lives on.
It is illegal to buy or sell human organs or tissues. Any financial incentive or profit relating to tissue/organ donation is excluded and will be penalized.
The main religions have a favourable view on the matter, for example, the Catholic and Protestant Churches, and the Hebrew, Buddhist, Hindu and Islamic Religions and classifies donation as an act of charity.
First of all, you need to let your family know about your willingness to be a donor after death i.e. that you have decided that you wants to help a fellow human being after death. Consent to donate will be requested, following death, also from those of your next-of-kin who are legally entitled to give consent, by medical staff or by the local Transplant Coordination/Procurement Unit.
Spare your family this difficult decision and make your own decision while you are still alive. Obtain, complete a donor card, or register with your local/regional/national donor registry, in order to freely decide which organs or tissues you would like to donate after your death. Make sure to inform your family of this decision.
Light up the world even after your death – say YES to eye donation.
Almost anyone – age does not play a role in eye donation. Theoretically every deceased person is a potential donor.
As with other forms of donation, a person must be screened to exclude highly communicable diseases and other medical disorders which may affect the safety or quality of the donated tissue. People with cancers (except leukaemia and lymphoma), heart disease, respiratory disease, and diabetes can be eye donors. Most eye problems not involving the cornea will be suitable e.g. glaucoma, previous cataract surgery, retinopathy, vision problems requiring glasses or contact lenses.
In contrast to solid organs a cornea can be removed up to 24 hours after the ascertainment of death.
There is no substitute for human tissue. The transplantation process depends upon the precious gift of eye donation from one person to another.
If determined to be suitable by medical staff or transplant/procurement coordinators, the family of the deceased can be approached with the option to donate the eyes. Consent is always required from one’s next-of-kin, so it is important that people discuss their wishes with their families.
Donation does not disrupt funeral arrangements as eye tissue procurement occurs within 24 hours of death. Families may proceed with funeral arrangements without delay or interruption
There is no visible difference to appearance to the deceased person after eye retrieval, so that the family can say goodbye afterwards. The donor’s body is treated with respect at all times and the skilled tissue retrie val team will perform the surgical eye- or corneal- retrieval procedure, which is designed to maintain the natural appearance of the donor, so as to preserve the person´s integrity.
val team will perform the surgical eye- or corneal- retrieval procedure, which is designed to maintain the natural appearance of the donor, so as to preserve the person´s integrity.
Various tests and evaluations need to occur, but the vast majority of tissue is suitable for transplant. Tissue that does not meet the criteria for transplant can be used for valuable research or teaching purposes where appropriate and when consent has been given for non-therapeutic use.
Although the whole eye cannot be transplanted, both the cornea and sclera can be utilised separately for ocular surgery. However, the entire eye may be used for research and educational purposes.
NO. As certain medical conditions pose a problem for transplantation and a potential danger for the recipient, an extensive review of the donor’s medical, family and social history is conducted by the eye bank, as well as detailed examinations of the donor eyes in order to ensure that the donor cornea is functional. Efforts are made to utilise those donated eyes which are rejected as unsuitable for transplantation for research, training and educational purposes, where appropriate and when consent has been given for non-therapeutic use.
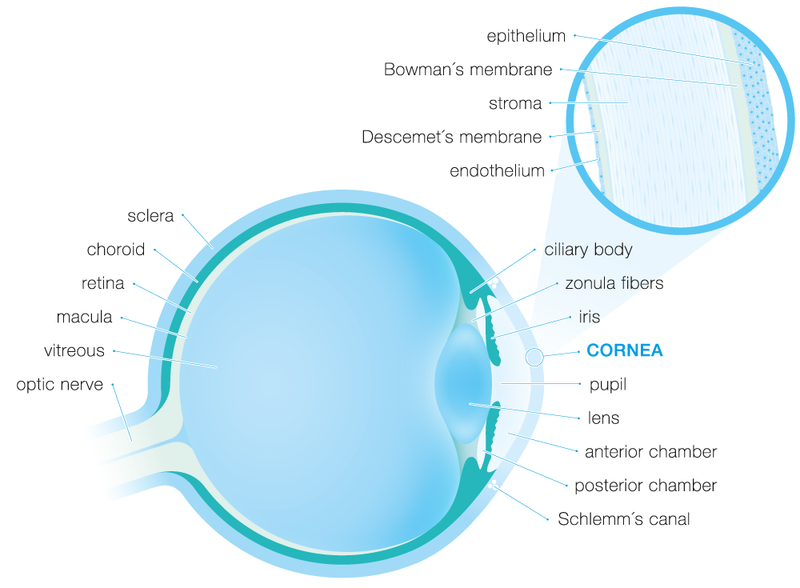
The cornea is the crystal clear window in the front of the eye which reveals the coloured iris and the black pupil. Microscopically it is composed of 5 distinct layers, each of which fulfils a specific function. Furthermore, its surface is coated with an ultra-thin liquid film, the tear film.
The epithelium is the outer protective cell layer of the cornea. It is only about 5-6 cell layers thick and, similarly to the upper skin layers, quickly regenerates when the cornea is injured. If the injury penetrates more deeply into the cornea, it may leave a scar. Scars leave opaque areas, causing the corneal to lose its clarity and sheen.
The Bowman's layer lies just beneath the epithelium. Because this layer is very tough and difficult to penetrate, it protects the cornea from injury.
The stroma is the thickest layer and lies just beneath Bowman's. It is composed of tiny collagen fibrils that run parallel to each other. This special formation of the collagen fibrils gives the cornea its clarity.
The Descemet's membrane lies between the stroma and the endothelium.
The endothelium is just underneath the Descemet's membrane and is only one cell layer thick. This layer pumps excess liquid out of the cornea and in this way precisely maintain the moisture content that is required to ensure a perfect transparency. To ensure this function, not even the tiniest gap may originate in this cell layer. If endothelial cells are lost, the remaining cells have to enlarge to cover the originating gap, since endothelial cells are unable to propagate or regenerate.
The cornea has three major functions.