

To be functional, the cornea must remain transparent and rounded in shape. When the cornea is no longer able to adequately accomplish one or more of its functions (transparency, focused imaging, stability) and no other therapies are possible, the only available treatment is the transplantation of a clear human cornea. At present no effective artificial cornea exists, unlike modern artificial lenses, and therefore a viable cornea from a recently-deceased person is the only therapeutic option available. Without a transplant, many of these patients would become blind or severely visually-impaired.
The most frequent corneal pathologies relate to the abnormal curvature and deformation of the cornea, with keratoconus as the best known example.
Another frequent cause for corneal transplantation is corneal cloudiness. Cloudiness can occur for many reasons: if the corneal endothelium fails, the cornea swells due to the excess permeation of moisture and exhibits a milky haze.
Another reason may be opacification due to scars, for example after injuries, chemical burn, thermal burn, infection or ulceration. Also certain hereditary diseases and metabolic diseases may lead to opacification. If a cornea develops non-healing defects under certain circumstances, transplantation may be the only effective treatment in single cases.
If a cornea melts due to certain diseases or infections, an immediate emergency corneal transplantation may become necessary.
The first corneal transplant was performed in Olomouc, Moravia, (Czech Republic) on 7 December 1905 and, successively, has become one of the most frequent types of transplantation performed worldwide, benefitting patients ranging in age from new-born to 104 years old. Furthermore, the procedure is relatively straightforward and usually takes no more than an hour to complete. It is generally unproblematic, and complications are extremely rare.
Every corneal transplant (keratoplasty) is a microsurgical operation, performed with the aid of an operating microscope. The surgeon removes the central part of the diseased or damaged cornea and replaces it with a healthy cornea from a donor. Stitches are applied with a suture thinner than a human hair. The procedure lasts from 30 minutes to an hour and a half, according to the different transplant options available, and can be done under general or local anaesthesia or local, depending on the patient's needs and habits of the surgeon.
A successful corneal transplant results in a gradual improvement in vision. There is often useful vision within a few weeks. However, in some cases, it may take several months to a year for full vision to develop.
The corneal transplant surgery is generally performed on an outpatient basis. Most patients enter the hospital or surgery centre a few hours prior to surgery and leave that same day.
Compared to the transplantation of solid organs, corneal transplantation shows a considerably high success rate. This success rate has much to do with the special biological nature of the cornea itself, along with the remarkable improvements in microsurgical techniques and therapeutic treatments, which makes it less prone than other organs to “rejection”, which is the body´s immune defence.
The low rejection rate and relative absence of systemic disease transmitted through transplanted corneas is known to be attributable to the “privileged” nature of corneas; the medical literature often refers to the cornea as “privileged’ because of the absence of blood vessels that in other anatomical sites transport antigens and pathogens from donor to recipient, therefore in most cases a systemic immunosuppression is not necessary.
Nevertheless, a corneal transplantation bears a higher risk than other ophthalmic surgeries, given that it involves the grafting of a non-histocompatible tissue.
The type of transplant performed is usually determined by the corneal pathology of the recipient, and the quality of the replacement tissue available. Corneal transplant procedures include standard penetrating keratoplasty, femto keratoplasty, posterior lamellar keratoplasty and anterior lamellar keratoplasty.
The clinical indications may be visual, structural, therapeutic, cosmetic or a combination and the operating surgeon will inform one about the risks and benefits of the various options available.
The success of a corneal transplant can be defined as better vision, less pain, comfortable spectacle or contact lens wear, reduced glare and, most importantly, an improved quality of life.
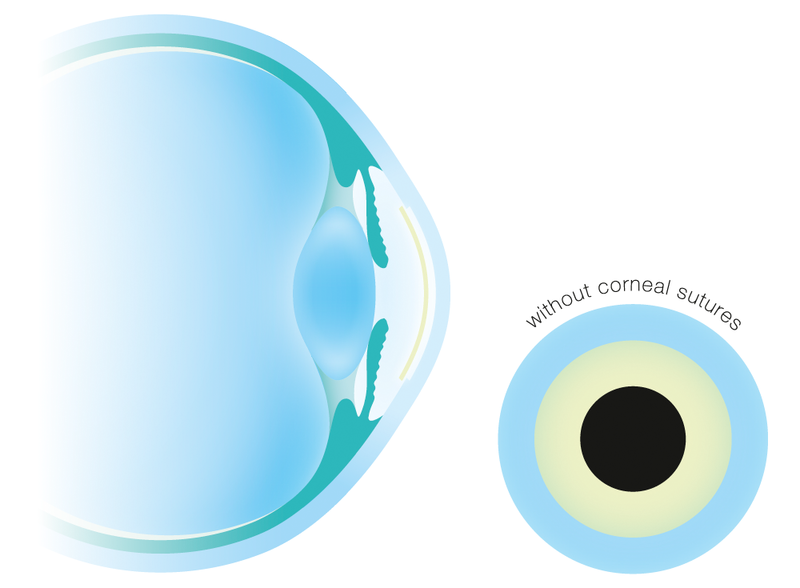
 Penetrating (full thickness) keratoplasty involves transplanting all the layers of the donor cornea. In this procedure a circular disk of the diseased cornea is removed under the surgical microscope with the help of a special instrument called a trephine. A disk of the donor cornea is prepared which precisely matches the size and sutured in the created aperture in the recipient eye with the help of fine sutures.
Penetrating (full thickness) keratoplasty involves transplanting all the layers of the donor cornea. In this procedure a circular disk of the diseased cornea is removed under the surgical microscope with the help of a special instrument called a trephine. A disk of the donor cornea is prepared which precisely matches the size and sutured in the created aperture in the recipient eye with the help of fine sutures.
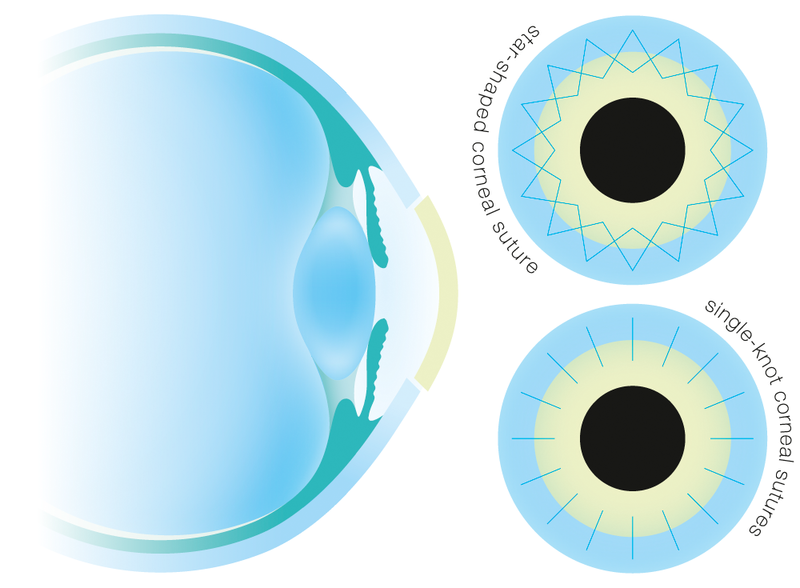
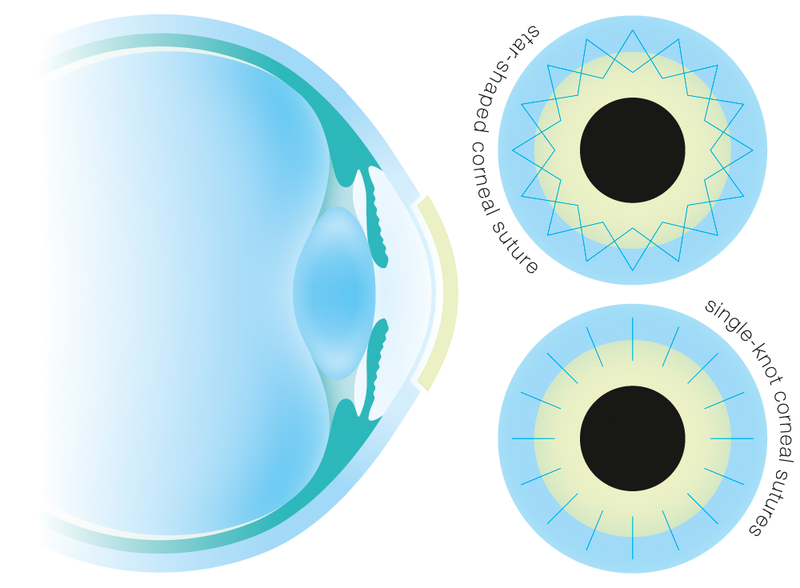
Whether the transplant is sutured with two star-shaped continuous sutures or an appropriate number of single-knot sutures is the decision of the surgeon depending on the circumstances of the individual case. The sutures used are made of nylon and are several times thinner than a human hair.
As the full-thickness of the recipient’s cornea is replaced during the transplant, this type of keratoplasty is the most invasive as it involves an intraocular “open sky” surgical procedure. Consequently, the transplant is more prone to immunological rejection and graft failure.
The most recent technical advancement involves the removal of the diseased tissue and of the transplant with a so-called Femtosecond laser. Since the laser can only cut through clear tissue, this method cannot be applied in all cases. Also, this method is not recommendable for strongly deformed corneas for technical reasons.
 In inner layer transplantation (posterior lamellar or endothelial keratoplasty, Descemet´s stripping automated endothelial keratoplasty = DSAEK or Descemet´s membrane endothelial keratoplasty = DMEK) the defective endothelium of the diseased eye including the Descemet´s membrane is circularly cut, separated, removed and replaced with a corresponding lamella or disk of healthy donor tissue.
In inner layer transplantation (posterior lamellar or endothelial keratoplasty, Descemet´s stripping automated endothelial keratoplasty = DSAEK or Descemet´s membrane endothelial keratoplasty = DMEK) the defective endothelium of the diseased eye including the Descemet´s membrane is circularly cut, separated, removed and replaced with a corresponding lamella or disk of healthy donor tissue.
The rolled donor corneal disk is inserted into the eye through a small lateral incision. The graft tissue is unfolded inside the eye and is then pressed against the corneal bed and kept in place at the intended position with an air bubble. There it adheres, whilst the air bubble is absorbed and dissolves within several days.
To avoid a so-called pupillary block with massive intraocular pressure increase due to the air inside the eye, a small opening in the iris (iridectomy) is created during surgery from many surgeons. In the case of inner layer transplantation the patient must remain in supine position 24 hours after surgery, so that the air bubble inside the eye can press the transplant against the bed, thus ensuring adhesion.
Today this method has increasingly become the method of choice in the relatively frequent corneal opacifications due to failure of the innermost cell layer (endothelium) regardless of its cause, if the remaining corneal layers do not exhibit pathological changes. In many cases the operation is combined with cataract surgery.
 With outer layer transplantation (anterior deep lamellar transplantation, deep anterior lamellar keratoplasty = DALK) the anterior corneal layers are separated from the Descemet´s membrane and the endothelium, removed and replaced with the same layers from the donor cornea. In this case the transplant needs to be fixed with fine sutures, like in penetrating keratoplasty.
With outer layer transplantation (anterior deep lamellar transplantation, deep anterior lamellar keratoplasty = DALK) the anterior corneal layers are separated from the Descemet´s membrane and the endothelium, removed and replaced with the same layers from the donor cornea. In this case the transplant needs to be fixed with fine sutures, like in penetrating keratoplasty.
This technique is preferred in cases which are limited to pathological changes of the anterior corneal layers and when the two innermost corneal layers (Descemet´s membrane and endothelium) are perfectly healthy.
This surgical procedure, even though planned, cannot always be reliably performed, with the result that the surgeon in some cases has to switch to a penetrating keratoplasty intra-operatively which is possible without any problems.
Although, the technical details of the lamellar operating techniques are in constant and rapid evolution – the principles of anterior and posterior lamellar surgery techniques are now well-established and remain mostly unchanged.
Descemet’s stripping endothelial keratoplasty and deep anterior lamellar keratoplasty are now being used worldwide as first-line treatments, and more sophisticated developments, such as Descemet’s membrane endothelial keratoplasty and femtosecond-assisted anterior lamellar keratoplasty, are gaining popularity.
The main advantage of selective lamellar techniques, both anterior and posterior, over the older and more traditional penetrating keratoplasty procedure, is that they lead to less invasive surgery and a much lower rejection rate as there is a significant reduction in the damage to the eye, given that the anatomy and strength of the eye is preserved. Because they are partially extra-ocular procedures, they also avoid most of the complications associated with intraocular “open sky” surgery. In addition, anterior techniques have the specific advantage of preserving the endothelium, thus greatly reducing the risk of immunological rejection and graft failure. Rejection episodes, which are mainly related to the endothelium, are now infrequent.
Total cornea transplant recovery time can be up to a year or longer. Vision will be blurry for the first few months — and in some cases may be worse than it was before — while the eye gets used to its new cornea.
Spectacle glass needed for best correction of the visual acuity after corneal transplantation may completely differ from that used preoperatively. Within the first weeks and months these values are still subject to change in many cases.
The fine sutures used for suturing of the cornea (in case of a penetrating as well as anterior lamellar keratoplasty) must remain in the eye for a number of months, in some cases for up to 1 – 2 years. Adjustments can be made to the sutures surrounding the new corneal tissue to help reduce the amount of astigmatism resulting from an irregular eye surface.
As vision improves, gradually one will be able to return to their normal daily activities. For the first several weeks, heavy exercise and lifting are prohibited. However, one should be able to return to work within a week after surgery, depending on the specific type of job and how quickly vision improves.
Steroid eye drops will be prescribed for several months to help one’s body accept the new corneal graft, as well as other medications to help control infection, discomfort and swelling. The operated eye should be protected at all times by wearing a shield or a pair of eyeglasses so that nothing inadvertently bumps or enters into the eye.
As with any type of surgery, patients are recommended to follow the precise instructions of their eye surgeon in order to help minimize corneal transplant complications and expedite healing.
An area of great advancement is corneal restoration by cell therapy and tissue engineering. Today it is possible to expand cells in the laboratory and transfer them to the diseased cornea to restore structural integrity and transparency. Surface reconstruction by autologous limbal epithelial stem cell transplantation is a proven concept, and endothelial cell transplantation is increasingly becoming a reality.
In the near future, regenerative medicine and innovative corneal surgery will be successfully combined and it is possible to foresee new surgical strategies — DMEK or DALK — with tissue-engineered grafts. The next step will be an artificial cornea made with autologous (means patients own cells) cultured cells. In this exciting innovation process, eye banks are playing a central role in ensuring that basic research is able to step from bench to bedside.